Meet Our Research Team
Salvatore Dimauro, MD | Don Mahuran, PhD/Michael Tropak, PhD | Fanny Mochel, MD | Pablo Escribá, PhD | Wyatt Yue
Adult Polyglucosan Body Disease (APBD) is a disease in which long chains of sugars, called polyglucosans, accumulate in nerve cells where the activity of an enzyme called Glycogen Branching Enzyme 1 (GBE1) is low. It is hypothesized that these polyglucosan bodies injure nerve cells and their formation reduces the body’s energy supply. The abnormal glycogen that accumulates in APBD patients cannot be broken down to supply glucose (sugar) for energy to the cells.
Summaries of some of the research now being done on this disease are described below, together with biographical information on the Principal Investigators.
Alex Lossos, MD

Biography
Dr Lossos attended the Hebrew University of Jerusalem, where he obtained his MD degree from the Hadassah Medical School. He completed training in adult neurology at the Hadassah Medical Center and received the Faculty of Medicine award for excellence in clinical and basic research. He is board-certified in neurology. Since joining the senior staff of the Department of Neurology, Hadassah Medical Center in 1993, Dr. Lossos has lead a multidisciplinary adult neurometabolic and neurogenetic clinical and basic research group. He actively collaborates with multiple local and international medical centers and professional organizations. In 2006, Dr. Lossos was appointed Associate Professor in Neurology at the Hebrew University.
Research
Dr. Lossos’s research has focused on adult-onset neurometabolic disorders with particular interest in diagnosis, clinical phenotype, genotype-phenotype correlations, pathogenesis and possible therapeutic interventions. His pioneering studies in Adult Polyglucosan Body Disease (APBD) were acknowledged worldwide and led to the identification of the biochemical and molecular basis of the disease. He was also involved in investigation of hereditary leukoencephalopathies, Niemann-Pick disease type C, familial amyloid polyneuropathy, Sjögren Larsson syndrome, autosomal recessive myopathy with external ophthalmoplegia, chorea-acanthocytosis, and frontotemporal dementia. His ongoing projects include studies in hereditary spastic paraplegia and spinocerebellar ataxia and APBD. Dr. Lossos has authored many peer-reviewed publications and has presented his research at numerous national and international meetings. Dr. Lossos also works with Dr. Or Kakhlon, another Principal Investigator.(See below, for further discussion of their research.)
Applications of APBD research to other diseases
In many different genetic diseases, long chains of sugars, called glycogen, accumulate in cells forming aggregates which can injure them. In diseases affecting liver and muscle cells, the glycogen aggregates are wrapped in lipid membranes. However, when glycogen aggregates form in diseases affecting the nervous system, they are not associated with membranous structures inside cells. This difference may explain why strategies for treating glycogen aggregation diseases in the nervous system, as opposed to non-neurological diseases, do not involve attempts at clearing intracellular membranous structures. Our project will seek ways in which biological pathways, already active in nerve cells, can be utilized to clear the nerve cells of glycogen aggregates. The rationale of our approach is that enhancement of a biological process already functioning in the cell may constitute a more efficient way of clearing glycogen aggregates, regardless of whether such a process involves segregation of the aggregates in membranous structures.
In our research so far, we have developed a cell model for the onset of APBD, based on silencing GBE1 in nerve cells using specific short RNA sequences. We intend to use it to test whether enhancement of the following processes, typically active in nerve cells, can reduce toxicity associated with glycogen aggregation:
a. Autophagy, in which membranes engulf components inside cells and degrade them.
b. Interaction between glycogen aggregates and special filaments inside the cells called microtubules, which might transport the aggregates out of the cells. c. Inhibition of an enzyme called glycogen synthase which synthesizes glycogen and can therefore lead to its unwanted accumulation. (Glycogen synthase is normally inhibited in neurons. However, this inhibition is restricted in some neurological diseases involving glycogen aggregation, such as in Lafora disease.)
Approaches shown to reduce the toxicity of glycogen aggregation could potentially be used to treat numerous neurological diseases, as well as aging per se, where glycogen aggregation is observed. This applies not only to typical neurological disorders involving glycogen aggregation such as Adult Polyglucosan Body Disease (APBD) and the Lafora disease, but also to well-studied neurological disorders such as Alzheimer’s Disease, where glycogen aggregation has been observed in nerve cells.
Berge Minassian, MD
 Biography
Biography
Dr. Berge Minassian is a neurologist and senior scientist at the Hospital for Sick Children and the University of Toronto in Toronto, Canada. He graduated from McGill Medical School in Montreal, trained in adult neurology at the University of California, Los Angeles and in pediatric epileptology at The Hospital for Sick Children, Toronto.
Dr. Minassian has had a longstanding interest in two diseases in which polyglucosans form. Lafora disease a progressive myoclonus epilepsy, which is fatal disease affecting children and Adult Polyglucosan Body Disease (APBD). Dr. Minassian’s main goal is to acquire the knowledge of how polyglucosans form in the brain and how to remove them in order to cure patients. His lab has discovered the genes for Lafora disease and are using molecular knowledge of the two diseases to reconstruct the understanding of polyglucosan formation and find ways to eliminate it.
Research
Arresting APBD by downregulating Glycogen Synthase (GS)
In downregulation a cell decreases the quantity of a cellular component, such as RNA or protein, in response to an external variable. In our research on Lafora disease, we showed that downregulating glycogen synthesis through removing the GS activator PTG in mice enabled us to stop all polyglucosan formation. There were practically no further polyglucosan bodies, gliosis disappeared, neuronal death disappeared, and the seizures that characterize that disease disappeared (Turnbull et al., 2011).
We have since followed these mice well into old age, over two years, and they remain absolutely healthy. One crucial insight from this study is that removal of polyglucosans and polyglucosan bodies cures the disease, showing that these abnormal structures that invade neurons actually cause the disease and that their elimination corrects the disease. At this point, if we can find a small molecule medication that inhibits GS safely, we will have a treatment for Lafora disease. We hope that by arresting the disease through preventing the addition of any further polyglucosans and eliminating a net accumulation over time, the body might be able to rid itself of already accumulated polyglucosans. Stopping the disease may therefore be not only a treatment, but a cure as well.
We now wish to precisely replicate the above study for APBD, following the same procedures and exactly the same experimental protocol. We will generate mice called double knockouts where the GBE1 Gene and PTG are inoperative. We will then study glycogen quantities and polyglucosans in these mice when they are six months old to determine whether we were able to eliminate polyglucosans. If we are successful, it will show that APBD is amenable to the same treatment as Lafora, once a small molecule is identified.
Eliminating polyglucosans from the APBD mouse brain by activating the protein amylase in neurons
We previously generated mice that produce amylase in neurons after feeding them the trigger molecule doxycycline. This work was done through APBDRF funding. Now that we have the APBD mice, we are breeding the amylase mice with the APBD mice. At six months of age we will activate amylase production and determine whether we are able to clear polyglucosan bodies from the APBD mouse brain. If this is successful, it will be both a treatment and a cure for the disease, reversing the lifelong accumulation of polyglucosans. This will open the door to a definitive treatment of APBD. We would look for a way to get amylase into neurons. Because APBD is a disease of later adult years, if we can reverse the polyglucosan accumulations at age 50, it will be a cure for the subsequent 50 years.
There is a very important financial advantage to doing the above two experiments simultaneously in terms of mouse cage costs and manpower. Both experiments will be completed within one year.
Turnbull J, Depaoli-Roach A.A, Zhao X, et al. (2011). PTG depletion removes Lafora bodies and rescues the fatal epilepsy of Lafora Disease. PLoS Genet 7, e1002037.
Or Kakhlon, PhD
 Biography
Biography
Dr. Kakhlon obtained his PhD (summa cum laude) from the Hebrew University of Jerusalem, where he graduated in 2002. Following his PhD, under the joint supervision of Prof. Z. Loav Cabantchik and Prof. Yosef Gruenbaum, he conducted his postdoctoral research at Dr. Sharon Tooze’s secretory pathways laboratory in Cancer Research UK, London. After his postdoc, he received a grant-funded research position at the Hebrew University of Jerusalem. Since January 2010, Dr. Kakhlon has been with the Department of Neurology at the Hadassah-Hebrew University Medical Center in Jerusalem where he studies APBD. Dr. Kakhlon is the author of 12 peer-reviewed publications. He has presented his work throughout his career in numerous scientific meetings.
Research
Knockdown of glycogen synthase (GS) and protein targeting to glycogen (PTG) by antisense oligos and triple-helix-forming oligos
The rationale behind these approaches is that knocking down enzymes which elongate glycogen chains is expected to reduce the formation of new polyglucosans, the abnormal and practically only form of glycogen generated in the neurons of APBD patients. Once no new polyglucosans are generated, the progress of the disease is expected to be in check, and patients’ condition might even improve if the pre-existing polyglucosans are slowly degraded.
Our knockdown targets are the glycogen synthesizing enzymes: glycogen synthase (GS), which “strings” glucose to form linear chains, and protein targeting to glycogen (PTG), a scaffold protein enabling the activation of glycogen synthase and its docking to glycogen. To knockdown GS and PTG we use 2 approaches:
1. Antisense oligonucleotides (ASO). These are small sequences of single-stranded DNA which bind specifically to an RNA target and prevent its translation into the specific protein it encodes. These ASOs are then injected directly into the brain where they can efficiently and specifically knock down their target. ISIS Pharmaceuticals has already screened and scaled up the ASOs and are currently performing tolerability studies for their injection to APBD mouse models generated by Dr. Akman and Lafora Disease mouse models generated by Dr. Minassian.
2. Triple-helix-forming oligos (TFO). These are computationally-designed peptide-nucleic acid based polymers which are very stable and bind very specifically to the DNA sequence they target. TFO are going to be used in the same way ASO will be used. The only difference is that they are inherently more stable and specific than ASO. We are currently testing TFOs for permeability into the nucleus. So far, it could not be convincingly demonstrated that the TFOs are internalized to the neurons nuclei (as opposed to yeast nuclei). We are currently working, in collaboration with the Israeli company GeneArrest, on ways to improve the nuclear permeability of TFOs.
High Throughput Screening of small molecules
This is a non-targeted approach where we screen tens of thousands of small molecules designed by computational chemists to be “druggable” (i.e., stable, predicted to dock to protein surfaces, soluble etc.). These molecules are being screened both by Dr. Akman and by Dr. Kakhlon for their capacity to reduce polyglucosan levels, readily detectable by periodic acid-Schiff reagent staining. The small molecules are screened on three models – mouse embryonic fibroblasts and brain cultures from APBD mouse models generated by Dr. Akman and skin fibroblasts from APBD patients. The purpose of using more than one model is the validation of positive hits.
Positive hits (some have already been found by Dr. Akman) are being analyzed by the computational chemist Dr. Dima Kozakov from Boston University in order to both find a chemical common denominator for all of them (a pharmacophore) and try to improve them by modifying their chemistry.
Computational peptide design
The computational chemist Amit Michaeli from the Hebrew University is designing peptides (amino acid compounds) that can either 1) bind to the mutated Glycogen Branching Enzyme (GBE) and stabilize it, or 2) destabilize the enzyme Glycogen Synthase (GS) which leads to unwanted glycogen accumulation.
We plan to test the effects of GS destabilizing and GBE stabilizing peptides on GS and GBE activities, respectively. We would also like to test whether peptides predicted to stabilize GBE affect its ability to resist change in its chemical or physical structure at high relative temperatures, as tested by Dr. Tropack. If, in response to heating, GBE Y329S would unfold at a higher temperature when exposed to a designed peptide or a pharmacological chaperone (a small molecule that stabilizes a folded protein), this would indicate that they can potentially stabilize GBE and thus counter the effect of the Y329S mutation.
Updates
a. In collaboration with Wyatt Yue and Amit Michaeli, we have used rational peptide design and discovered a novel tetrapeptide demonstrated to stabilize GBE Y329S. We are now writing this paper which should be submitted shortly. These data will be presented by Wyatt and myself in the meeting.
b. As you know, we have confirmed Dr. Akman’s discovery of the new manifesting heterozygous GBE mutation. Most of the work prior to the confirmation of Dr. Akman’s finding concentrated on exhausting all other possibilities for finding a new mutation. I guess Dr. Akman will be presenting this data and I can show some of my auxiliary findings.
c. I hope to test some of the rationally designed lipids, which I am supposed to receive from Dr Escriba, and show their effect on GBE activity. So far I have confirmed the activity of the recombinant enzymes he had sent me, which is also data I plan to show
d. I have tested the mechanism of action of some of the positive hits discovered in the High Throughput Screenings. These hits in most cases are GS inhibitors. I plan to discuss these results.
e. Lastly, I will present the High Throughput Screenings results we have so far. Positive hits from different libraries keep accruing and I will discuss these findings as well.
H. Orhan Akman, PhD
 Biography
Biography
Dr. Akman graduated from the Department of Biology Faculty of Arts and Sciences at Middle East Technical University in Ankara, Turkey. He continued his graduate studies at the State University of New York Health Science Center at Brooklyn, Brooklyn NY and graduated in 2002. He did his postdoctoral training for one year at Beth Israel Deaconess Medical Center, Department of Medicine at Harvard Institutes of Medicine. He continued his post graduate training at Columbia University in the laboratory of Dr Salvatore DiMauro. His project, titled, Generation and Characterization of Adult Polyglucosan Body Disease was funded by APBD Research Foundation in 2007. From September 2008 through 2011, he continued his research as an Instructor at Baylor College of Medicine, Houston, Texas. He is currently an associate research scientist at Columbia University Medical Center in New York, NY where he is developing an animal model for Adult Polyglucosan Body Disease (APBD).
Research
Animal models are very important in understanding the mechanism of diseases. They provide not only information about the course of the disease from womb to adulthood, but also are the best tool to test therapeutic approaches. Our research is concentrated on the development of a mouse model for APBD. We have introduced a human mutation into a mouse genome that targets the gene which is responsible for the proper synthesis of glycogen. Our preliminary data showed a direct correlation between the genetic mutation and APBD. We will further use this animal model to test certain pharmaceuticals and modified diets to cure eliminate the symptoms of APBD. Our research was funded initially by APBD Research Foundation, and currently by the Muscular Dystrophy Association (MDA).
Videos
https://www.apbdrf.org/resources/videos/scientists-speak
CV
Raphael Schiffmann, MD, MHS
 Biography
Biography
Dr. Schiffmann attended the University of Liège, Belgium where he obtained his M.D. degree cum laude. He completed training in pediatrics at the Shaare Zedek Medical Center in Jerusalem, Israel and in pediatric neurology at the Boston City Hospital and Tufts New England Medical Center Hospitals (Boston Floating Hospital). He is specialty board-certified in both pediatrics and pediatric neurology. After two and a half years as a staff pediatric neurologist at Hadassah University Medical Center, Jerusalem, Israel, he joined the National Institutes of Health. Between 1996 and 2007 he was the Lead Investigator directing the clinical research efforts of the Developmental and Metabolic Neurology Branch in the National Institute of Neurological Disorders and Stroke, National Institutes of Health. In December 2000, he received the degree of Master of Health Science in Clinical Research from Duke University. He is currently the Director of Baylor Institute of Metabolic Disease at the Baylor Research Institute in Dallas, Texas.
Dr. Schiffmann’s research has focused on neurogenetic disorders, and in particular on lysosomal storage diseases, making him a nationally and internationally recognized expert. He investigated the natural history, pathogenesis and treatment of Fabry disease, including pivotal studies that lead to the approval of enzyme replacement therapy for this disorder in 45 countries. He received the Merit Award from the National Institute of Neurological Disorders and Stroke for these contributions. He also investigated the pathogenesis of the neurological and neuropathological aspects of Gaucher disease and their response to enzyme replacement therapy and substance reduction therapy. His studies on the neurogenetics of mucolipidosis type IV confirmed the clinical and biochemical homogeneity of this disease `provided an important step toward identifying the mucolipidosis IV gene. He discovered three new leukodystrophy syndromes including Childhood Ataxia with Central Nervous System Hypomyelination (CACH), which is now recognized as one of the most common leukodystrophies. Dr. Schiffmann has authored 169 peer-reviewed publications, 20 reviews and book chapters and has presented his research in numerous national and international meetings.
Research
Institute of Metabolic Disease, Baylor Research Institute, Dallas, Texas
We are conducting a study in patients with APBD associated with glycogen brancher enzyme deficiency. We think that an insufficient supply of energy from glycogen to brain cells is a likely cause of APBD. The role of glycogen in the body is to supply energy. However, the abnormal glycogen that accumulates in patients with APBD cannot be broken down to supply energy to the cells.
The treatment being tested is an oil called triheptanoin or C7 which we hope will supply energy to brain cells instead of the glycogen. In an initial study, five patients showed stability or improvement in their ability to walk while taking C7. Based on these results we are now conducting a double-blind randomized controlled trial to compare C7 oil with regular vegetable oil in at least 18 patients. This 3-year study will be conducted in Dallas, Texas with sites in Israel and France. It is funded by the Baylor Research Institute and is the only APBD patient trial at this time.
Salvatore Dimauro, MD

Biography
Dr. DiMauro attended the University of Padua, Italy, where he obtained his MD degree and completed training in Neurology. Between 1969 and 1974, he was a Postdoctoral Fellow, Instructor and Assistant Professor in the Department of Neurology at the University of Pennsylvania, Philadelphia. In 1974, he became Associate Professor at the Neurological Institute, Columbia University, New York and in 1978 he was named Co-Director of the H. Houston Merritt Clinical Research Center at Columbia. He served as Director of the H. Houston Merritt Center from 1999 to 2010. Dr DiMauro is currently the Lucy G. Moses Professor of Neurology at Columbia University.
Research
Biochemical and Molecular Diagnosis of Muscle Glycogenoses
At the H. Houston Merritt Clinical Research Center, we investigate inborn errors of energy metabolism leading to neuromuscular disorders. More generally, our Center provides biochemical and molecular diagnostic tests for most glycogen storage diseases. Correct diagnosis is important for genetic counseling, appropriate treatment when available, and rational dietary and exercise regimens.
Because of their high energy needs, muscle and nerve are especially vulnerable to genetic defects of metabolism. Adult Polyglucosan Body Disease (APBD) affects nerve and muscle in two ways. First, APBs are large inert intracellular particles that make it difficult for muscle to contract and for nerve to conduct sensory and motor signals. Second, the disorder interferes with the production of adequate glucose from glycogen stores.
We offer a diagnostic blood test for APBD which is accurate and does not require invasive muscle biopsy. Using a single blood sample, it is now possible to perform biochemical analysis, test for glycogen branching enzyme activity and perform DNA analysis and sequence the GBE gene.
Don Mahuran, PhD/Michael Tropak, PhD
Dr. Don Mahuran is a Senior Scientist in the Research Institute, Department of Genetics & Genome Biology, The Hospital for Sick Children (HSC) and a Professor in the Department of Laboratory Medicine and Pathobiology at the University of Toronto, Canada. He received his Ph.D. from the University of Windsor, Canada in 1976. He developed his long-term interest in lysosomal storage diseases during his postdoctoral training with Dr. “Sandy” Lowden, then head of the Division of Neurosciences at HSC from 1977-1980. In 1981 he left Canada to work with Dr. John Hopwood at the Adelaide Children’s Hospital in South Australia, returning to a staff position at HSC in 1982. Dr. Mahuran currently coordinates a group of eight Principal Investigators funded by a “Team” grant from the Canadian Institutes of Health Research (CIHR), whose goal is to develop small molecule-based therapeutics for lysosomal storage diseases.
Dr. Michael Tropak is a Research Associate in Dr. Mahuran’s Lab at the Research Institute, Department of Genetics & Genome Biology, The Hospital for Sick Children (HSC). He received his Ph.D. from the Department of Medical Genetics at the University of Toronto in 1996. His interest in glycosidases and lectins stemmed from his doctoral work on sialic acid lectins and sialidases in myelination and was solidified during his postdoctoral training with Jim Rini from 1997 to 2000 in the Department of Biochemistry at the University of Toronto. His attention and focus has once again returned to glycosidases in lysosomal storage disorders. He is also a Co-Investigator on the Team coordinated by Dr. Mahuran and funded by the CIHR.
Research
Identification of pharmacological chaperones that enhance the activity of glycogen branching enzyme in skin fibroblasts from patients with Adult Polyglucosan Body Disease
We propose to take a pharmacological chaperone (PC) approach to treating patients with APBD. PCs are small molecules that specifically bind to and stabilize the correctly folded, active form of the enzyme. This added degree of stability can off-set the destabilizing effects of certain types of mutations, increasing residual enzyme activity in cells and correcting the deficiency that results in APBD. To find drugs that act in this manner a “library” of chemical compounds that have already been used to treat other human disorders will be screened for those that stabilize the purified target enzyme (GBE) towards heating. This approach avoids the approximately $12 million dollar cost of the preclinical studies necessary to move a new drug into clinical trials.
We are now able to produce the human enzyme in bacteria and purify it. Using small amounts of this enzyme we have validated our screening approach with several compounds that are already known to bind and stabilize GBE, but for various reasons are not good drug candidates. The next funded steps in this project will involve 1) purifying large amounts of GBE, 2) Screening the library of compounds (approximately 2500) for drugs, “hits”, that can stabilize the enzyme towards heating, 3) confirming the activity of each hit in vitro, and 4) determining if any of the confirmed hits can increase GBE activity and protein levels in patient cells.
Our role in the screening can only begin after a sufficient amount of GBE is purified by our collaborators. If one or more hits are confirmed to be active in cultured patient cells, a future grant will be sought to fund their evaluation in the APBD mice Dr. Akman Orhan has developed.
Fanny Mochel, MD
 Dr. Mochel graduated from the Medical School of the University of Montpellier III, France in 2001 and received her Doctor of Medicine Degree (M.D.) from the University of Paris Descartes in France in 2005. She subsequently obtained an inter-university diploma in Inborn Errors of Metabolism in 2004 from the University of Paris Descartes and earned her Master’s Degree in Molecular and Cellular Biology from the University of Pierre and Marie Curie in Paris in 2006. Dr Mochel is board certified in genetics. She worked with Dr. Raphael Schiffmann as a research fellow at the Developmental and Metabolic Neurology Branch in the National Institute of Neurological Disorders and Stroke at the NIH. She currently works at the Department of Genetics at La Salpêtrière Hospital in Paris and is completing her PhD in neuroscience at the University of Pierre and Marie Curie. Dr. Mochel has authored more than 30 peer-reviewed publications, reviews and book chapters and has presented her research at numerous national and international meetings.
Dr. Mochel graduated from the Medical School of the University of Montpellier III, France in 2001 and received her Doctor of Medicine Degree (M.D.) from the University of Paris Descartes in France in 2005. She subsequently obtained an inter-university diploma in Inborn Errors of Metabolism in 2004 from the University of Paris Descartes and earned her Master’s Degree in Molecular and Cellular Biology from the University of Pierre and Marie Curie in Paris in 2006. Dr Mochel is board certified in genetics. She worked with Dr. Raphael Schiffmann as a research fellow at the Developmental and Metabolic Neurology Branch in the National Institute of Neurological Disorders and Stroke at the NIH. She currently works at the Department of Genetics at La Salpêtrière Hospital in Paris and is completing her PhD in neuroscience at the University of Pierre and Marie Curie. Dr. Mochel has authored more than 30 peer-reviewed publications, reviews and book chapters and has presented her research at numerous national and international meetings.
Research
Manifesting Heterozygotes in APBD
APBD is often caused by a deficiency of glycogen brancher enzyme. This disease is inherited by an autosomal recessive mode. This means that both copies (or alleles) of the brancher enzyme gene are mutated (have an error). Since we all have two copies of the brancher enzyme gene, both parents of an APBD patient are carriers (or heterozygotes) of a mutated copy but are not affected by the disease since the normal copy of the brancher enzyme gene protects them. In order to have APBD, both copies of the brancher enzyme have to be mutated. Therefore, APBD patients inherit one mutated copy from each parent.
The mutations in both copies of the brancher enzyme gene are identified in most APBD patients. However, using standard methods of gene sequencing, in about 40% of the patients we can identify only one mutation. A patient with this result is sometimes referred to as a ‘manifesting heterozygote’. However, such APBD patients have the same degree of brancher enzyme deficiency and the same disease severity as those with mutations of both copies of the gene identified.
Therefore, according to Dr Salvatore DiMauro’s work, we think that the other copy, or allele, of the brancher gene is also abnormal but the abnormality cannot be detected using the common sequencing techniques. The ‘mysterious’ abnormality of the other copy of the brancher enzyme gene can be either a complete absence (deletion) of the gene, a mutation in a part of the gene that controls transcription or more likely a mutation in a part of the gene that is responsible for the assembly of its messenger RNA. The messenger RNA is the nucleic acid that is “translated” by the cell to make the brancher enzyme protein. An incorrect assembly of the messenger RNA usually leads to absence of glycogen brancher enzyme produced by the affected copy of the gene.
My research has focused on neurogenetic and neurometabolic disorders. In particular, I have developed new biochemical diagnostic tools using nuclear magnetic resonance spectroscopy of body fluids in order to identify new complex neurological diseases or biomarkers for known neurological diseases. I have expertise on energy metabolism in the brain and have developed therapies addressing cerebral energy deficit in inborn errors of metabolism as well as neurodegenerative diseases such as Huntington disease.
Escribá, Pablo PhD
 Biography
Biography
With a PhD and a degree in Biology, Dr. Pablo Escribá moved from his hometown of Mallorca to New York to work at SUNY’s Neurobiology and Behavior Department. Dr. Escribá has worked in several labs and universities in the US, such as the Ann Smith Laboratory and the Medical University of South Carolina. In Europe, he has worked in Geneva, Switzerland, and in Mallorca. In 2006, he became a tenured professor at the Universidad de las Islas Baleares. He has been working in collaboration with the APBDRF since 2013.
Research history
Dr. Escribá’ s focus in the last 15 years has been on discovering the dynamic role of the cellular membrane in the different functions of the cell. Four molecules developed by him and his team have been selected for clinical tests on humans, making Dr. Escribá’s research team one of the most successful in the medical world. One of the molecules developed is about to be used for the treatment of neurodegenerative diseases. In 2013, Dr. Escribá and his team made significant advances in their research on molecules for the treatment of APBD, thanks to APBDRF support and the help of their collaborating scientists around the world. By the middle of 2014, they expect to be initiating studies on model systems of the disease.
Current research related to APBD
In Dr. Escribá’s words:
GBE1 protein takes two forms: the so-called wild type (normal GBE protein) and Y329S, the mutation found in many APBD patients. We are producing both types modified in a way that can be purified in high amounts. We use insect cells to over express these proteins in a way that resembles the human ones. We have observed that the mutated Y329S form of the protein binds well to membranes, which decreases its activity, whereas the wild type does not bind and is therefore available for normal activity.
We plan to distribute the protein to two other investigators, Or Kakhlon in Israel and Wyatt Yue in the UK, in order to investigate together the effect of different lipids on the structural and functional characterization of both forms of the enzyme. In addition, we have designed and are testing a number of molecules that may regulate GBE1-membrane interactions to increase the enzyme activity. Our goal is to find a potentially therapeutic molecule to be used in cellular and animal models of APBD and, eventually, in man. We know that triheptanoin is being studied for its effectiveness in reversing the symptoms associated with the condition. The results of this study will help in the designing of new molecules with potentially greater efficacy.
I am very glad to have the confidence and support of the APBDRF and I hope that the combined efforts of all the scientists in the field will bring, within this decade, a plausible treatment.
Wyatt Yue
 Biography
Biography
Wyatt Yue is a structural biologist trained from both academic and industrial background, with experience in studying diverse biology systems including membrane transport, chromatin modification, and human metabolism. Wyatt obtained a BA in Biochemistry at University of Oxford, and a PhD in Crystallography at Birkbeck College, University of London. He pursued a postdoc in Institute of Cancer Research with Laurence Pearl FRS, followed by a stint at the fragment-based drug discovery company Sareum Ltd. In 2008 he joined the Structural Genomics Consortium, University of Oxford, where he established the ‘Metabolism & Organelle Biogenesis’ group in 2011. His research interest is the use of structural, biochemical, and chemical biology approaches to study diverse metabolic protein families in the human genome. He collaborates with front line clinicians to understand the molecular basis of inherited metabolic disorders, and with drug developers to investigate the potentials of small molecule therapy for genetic diseases.
Research interest
Glycogen biosynthesis involves the priming enzyme glycogenin (GYG1/2), the elongation enzyme glycogen synthase (GYS1/2), and the branching enzyme (GBE1). Mutations on the GBE1 gene lead to the highly heterogeneous form of glycogen storage disorder type IV, including an allelic variant, adult polyglucosan body disease, a late-onset neurological disorder with a prevalent missense mutation p.Y329S. We have an ongoing interest in understanding the catalytic and disease mechanism of human GBE1. Our initial attempts to over-express human GBE1 in E. coli were unsuccessful. This was circumvented by the baculovirus-infected insect cell system, with which we have obtained soluble, recombinant GBE1 in wild-type and mutant forms, and determined its 3D crystal structure. Our long-term goal is to establish a molecular basis for disease-causing mutations (e.g. p.Y329S) and develop ‘pharmacological chaperones’ as novel therapeutics.
Updates
We thank the APBDRF for the generous funding support, allowing us to commence the GBE1 pharmacological chaperone project from September. We are currently preparing recombinant GBE1 samples to screen against several drug-like libraries (e.g. MicroSource Pharmakon, 1600 compounds; Sigma-Aldrich LOPAC, 1280 compounds; NIH Clinical Collection, 800 compounds), using the in vitro thermal shift assay. We are also comparing the biochemical and biophysical properties of mutant Y329S protein with wild-type in order to yield further insight into the molecular consequence of the Y329S mutation. The above work is performed by 15% FTE of a postdoctoral fellow.

 Biography
Biography Biography
Biography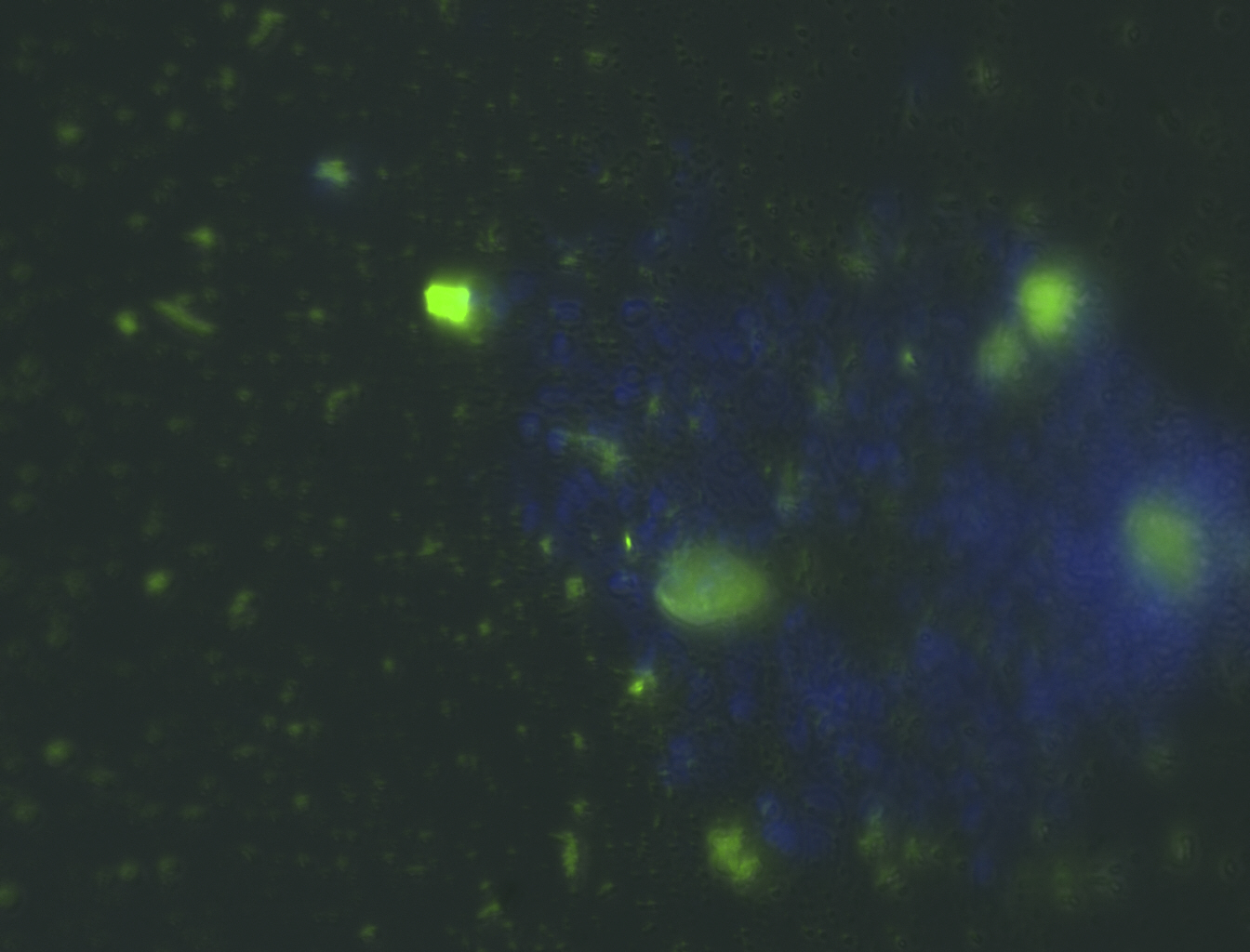
 Biography
Biography Biography
Biography